COPD Study Indicates Certain White Blood Cells May Predict Patients’ Response to Inhaled Corticosteroids
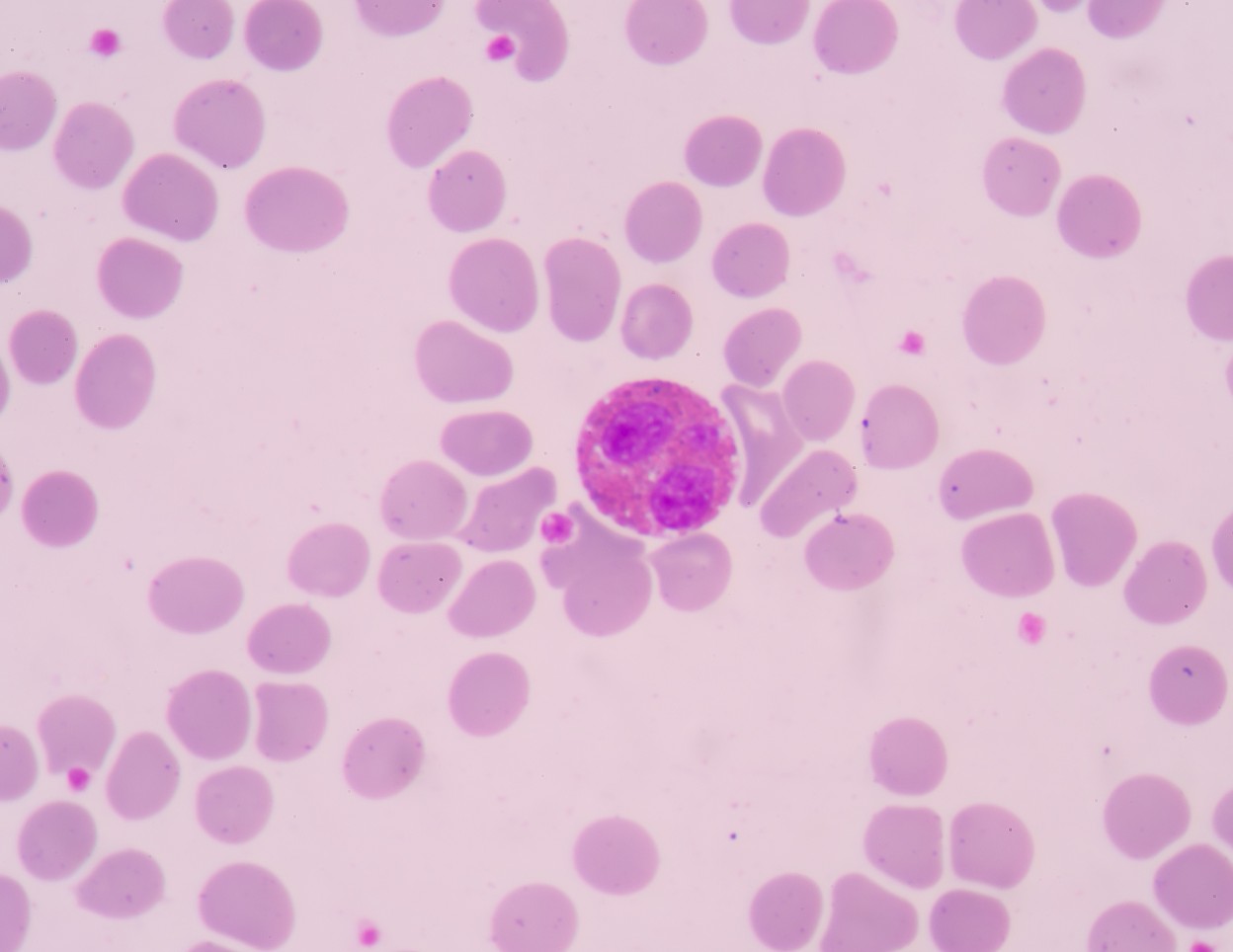
Boehringer Ingelheim recently announced the publication of a new research article detailing the measurement of specific white blood cells, called eosinophils, to prediction the response to inhaled corticosteroids (ICS) in patients with chronic obstructive pulmonary disease (COPD) and a history of exacerbations.
The study was developed using data from the WISDOM clinical trial, which included patients with severe to very severe COPD, and aimed to establish if there is a need for continuous treatment with an inhaled corticosteroid therapy on top of two potent long-acting bronchodilators — Spiriva and long-acting beta2-agonist (LABA).
The research article, “Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial,” was published in The Lancet Respiratory Medicine.
In the WISDOM trial (NCT00975195), 2,488 COPD patients received 18 μg of tiotropium, 100 μg of salmeterol, and 1,000 μg of fluticasone propionate daily for six weeks, and were then randomly assigned to receive either continued or reduced ICS over a period of 12 weeks. In the post-hoc analysis of the WISDOM trial, researchers evaluated the rate of exacerbations and timed exacerbations in relation to blood eosinophil levels.
The results indicated that only 20 percent of the patients benefited from ICS treatment on top of Spiriva and a LABA when it came to a reduction in the risk of exacerbations. The patients who benefited from a reduced exacerbation risk due to the continued use of ICS in addition to bronchodilators had higher levels of blood eosinophils (equal to or greater than 300 cells/µL; more than 4 percent). The increase in exacerbation rates became more apparent as the eosinophil cutoff level rose.
“Long acting bronchodilators are a mainstay therapy in COPD management; however, in clinical practice ICS is widely used across all COPD stages,” said study investigator Peter Calverley, professor of pulmonary and rehabilitation medicine at the University of Liverpool, in England, in a Boehringer Ingelheim press release.
“Previously, it has been difficult to determine the subset of patients who respond to ICS. These findings will help physicians more confidently identify which patients may benefit from ICS therapy, helping minimize exposure to the risk of side effects related to long-term ICS use,” Calverley said.
Researchers believe that, while further studies are needed for confirmation, the data suggests that eosinophil counts of 4 percent or greater, or 300 cells per μL or more, might identify a harmful effect of ICS withdrawal.





