Sensitization to a Fungus May Cause Bronchiectasis in Patients with COPD, Study Indicates
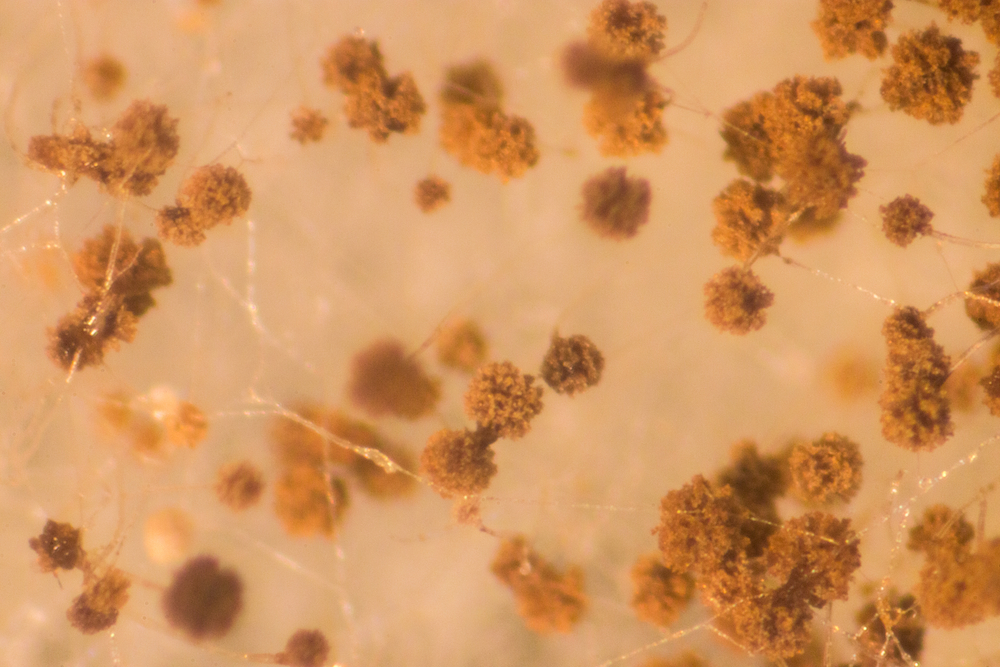
An allergic sensitization to the Aspergillus fumigatus fungus may lead to bronchiectasis in patients with chronic obstructive pulmonary disease (COPD), Belgian researchers suggest.
The study, “Sensitization to Aspergillus fumigatus as a risk factor for bronchiectasis in COPD,” was published in the International Journal of Chronic Obstructive Pulmonary Disease. The research was led by investigators at University Hospitals Leuven and KU Leuven in Belgium.
Earlier reports showed a greater prevalence of allergic sensitization to A. fumigatus in COPD patients, and its association with worsening lung function. Sensitization is defined as the presence of allergen-specific immunoglobulin (Ig) E — a type of antibody produced by the immune system in response to an allergy.
The overlap of bronchiectasis and COPD is a possible clinical condition. Bronchiectasis is a risk factor for mortality in COPD, and affects the safety and type of appropriate therapies. But the causes of bronchiectasis in patients with COPD were unclear.
Scientists hypothesized that sensitization to the mold A. fumigatus plays a key role in COPD-related bronchiectasis. They also studied whether vitamin D deficiency, often observed in patients with COPD and bronchiectasis, may contribute to A. fumigatus sensitivity.
Researchers evaluated sensitization to A. fumigatus in an outpatient clinical group of 300 COPD patients and 50 former smokers, used as controls. The scientists determined the prevalence of A. fumigatus sensitivity by measuring IgE levels. They also measured levels of vitamin D in the blood.
Results showed that approximately 18% of the COPD patients were sensitized to A. fumigatus, compared to only 4% of the controls. The presence of IgE specific to two A. fumigatus allergens (called f1 and f3) was associated with a 2.8-fold greater risk for bronchiectasis.
The results also indicated that most A. fumigatus-sensitized patients with COPD were males and had bronchiectasis.
Furthermore, these patients showed a greater incidence of P. aeruginosa and Serratia marcescens infections.
“This finding further emphasizes the clinical relevance of our results since these pathogens may play a role in exacerbations and can become multi-drug resistant,” the team wrote.
Concerning vitamin D, researchers found no correlation between vitamin D levels or cigarette smoke exposure with sensitization to A. fumigatus or bronchiectasis.
Overall, “these observations support the hypothesis that [A. fumigatus] hypersensitivity might contribute to the development of bronchiectasis in COPD,” the team wrote.
However, the researchers caution that the results do not confirm causality. “Because of the retrospective, observational design of this study, we were not able to demonstrate a causal relationship,” the team wrote. “Prospective, longitudinal studies are needed to prove causality and to allow speculation about preventive interventions.”
Future studies are warranted to unravel the mechanisms of the possible association between A. fumigatus colonization, sensitization, and bronchiectasis development.
“The search for underlying mechanisms in the development of bronchiectasis in COPD is relevant, since the presence of bronchiectasis in COPD influences management and prognosis of the disease,” the team concluded.





