Bronchiectasis in COPD Linked to Sinus Inflammation
Written by |
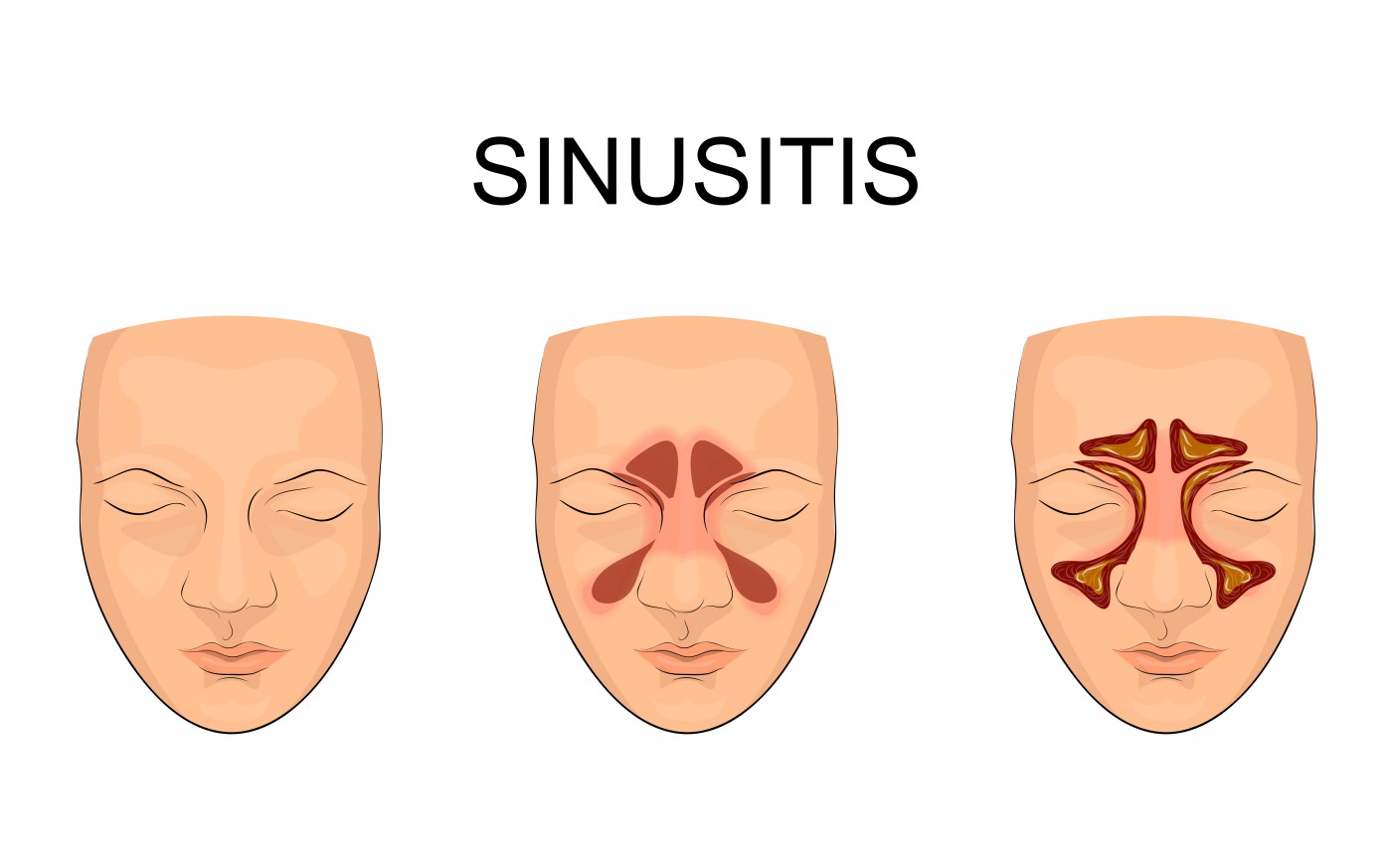
Chronic inflammation of the sinus cavities is more common among patients with chronic obstructive pulmonary disease (COPD) who also have bronchiectasis, underscoring the impact of chronic inflammation of the upper airways in more severe disease phases.
The study, “Chronic rhinosinusitis is associated with higher prevalence and severity of bronchiectasis in patients with COPD,” was published in the International Journal of COPD.
Earlier studies showed that chronic inflammation of the sinus cavities, called sinusitis, is linked to both COPD and bronchiectasis. But researchers at Beijing Tongren Hospital at the Capital Medical University in China, noted that not much is known about how such an inflammatory state impacts patients with both conditions.
The team then recruited 136 patients with stable COPD, and looked for the presence of both chronic sinus inflammation and bronchiectasis. The majority of the enrolled patients were in GOLD stages 2 and 3; only 5.9% had reached the most severe stage of COPD (stage 4). In the entire group, 66.2% were current smokers.
In the patient cohort analyzed, 48.5% had chronic sinus inflammation. There were more women among patients with sinusitis, and 57.6%of those with COPD and sinus problems also had bronchiectasis. Among COPD patients without this type of airway inflammation, only 37.1% had bronchiectasis.
Patients with COPD, bronchiectasis, and sinusitis also had more severe bronchiectasis than those without sinus inflammation.
But the inflammation did not affect only bronchiectasis. Researchers found that the more severe the sinus inflammation, the worse the COPD became, with lower forced expiratory volume in 1-second scores (FEV-1, a measure of lung function).
Not surprisingly, these patients also had higher levels of inflammatory factors in their sputum. In particular, researchers noted that inflammatory cells called eosinophils were more common in patients with sinus problems. They also noted that two cytokines (immune mediators), called IL-8 and MMP-9, were increased in COPD patients with bronchiectasis and sinusitis when compared with those without the inflammatory condition.
“We found that COPD patients with CRS [chronic rhinosinusitis] had a higher prevalence and severity of co-morbid bronchiectasis, which was associated with enhanced inflammation of the lower airways,” the team concluded.
In the study, researchers did not analyze the outcomes of the different patient groups, figuring that a study that follows patients over time would be more suitable for that purpose. Nevertheless, researchers pointed out that the data support the “united airways” concept — stating that upper airway disease is tightly linked to, and often precedes, diseases in the lower airways.