Strategy to Fight COPD-related Lung Inflammation Could Help Millions, Researchers Contend
Written by |
The blood growth factor called granulocyte-colony stimulating factor (G-CSF) underlies airway inflammation and lung tissue destruction in COPD, but also the symptoms in other tissues, including the heart and bone, a new study shows.
The findings of Australian scientists at Monash University and the University of Melbourne suggest that clinical therapeutic antibodies blocking G-CSF signaling — up to a point — are a potential therapeutic strategy for COPD.
“We found elevated levels of G-CSF in mice with COPD, and when it was eliminated, the excessive numbers of white blood cells in their lungs were markedly reduced and the lungs themselves no longer became diseased,” Margaret Hibbs, PhD, study lead author, said in a University of Melborne press release written by Andrew Trounson.
“Nothing previously has proved to be effective in treating patients with COPD, which is why this finding is so exciting. We can now attempt to target this protein,” she said.
The study reporting the findings, “Granulocyte-CSF links destructive inflammation and comorbidities in obstructive lung disease,” was published in the Journal of Clinical Investigation.
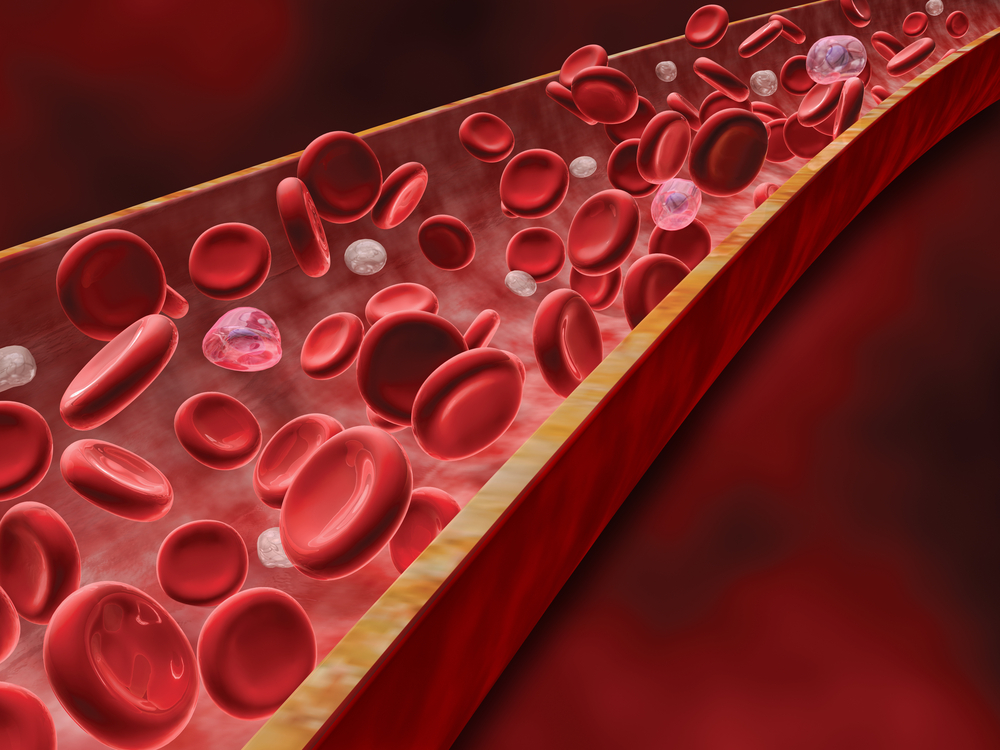
A study published in 2012 suggested that high numbers of cells of the immune system in the blood, especially the infection-fighting white blood cells, was associated with poor clinical outcomes in COPD. Follow-up studies strengthened this finding, offering evidence that high numbers of white blood cells in COPD are associated with damage to other tissues besides the lungs, including heart, muscles and bones.
Specialized white blood cells, called neutrophils and macrophages, are key combatants in lung infections. In COPD, they promote a pro-inflammatory state and contribute to tissue destruction.
“That really cemented in our minds that the white blood cells were a fundamental clue to follow,” said study author Gary Anderson, director of the Lung Health Research Centre at the University of Melbourne.
Following these studies, researchers decided to investigate the role of blood growth factors.
They focused on G-CSF, a blood growth factor required for the proliferation and differentiation of blood precursors of neutrophils, which are the most abundant type of white blood cells in most mammals.
To understand the role of G-CSF in COPD, researchers used mice deficient for the SHIP-1 protein, which spontaneously develop the typical symptoms of COPD, including inflammation, emphysema, and small airway fibrosis.
Deleting G-CSF in the SHIP-1–deficient COPD mice led to a marked reduction in airway inflammation and lung tissue destruction. Moreover, the signs of whole-body (systemic) inflammation were lessened in these animals, together with right heart hypertrophy, fat content, and bone osteoporosis.
“When we blocked G-CSF, the effect was absolutely striking,” said Anderson. “It prevented not only the emphysema, but also the wider medical problems, whether it be the heart, muscles or bone. We realized we had uncovered a potential pathway for treatments.”
While these findings were promising for potential therapeutic use, researchers had to make sure they could see the same in humans with COPD.
So, they teamed up with colleagues at the Royal Melbourne Hospital and confirmed that the bronchoalveolar lavage fluid of patients with COPD also had elevated G-CSF levels.
“We now have a very good case that we have indeed found a mechanism not just for preventing emphysema and chronic bronchitis in the lungs, but also for preventing the damaging medical conditions associated with it,” said Anderson. “There are several safe ways to reduce G-CSF in people and this concept can now be tested in human clinical trials.”
Clinical therapeutic antibodies that block G-CSF signaling can be dose-ranged to inhibit excessive production of G-CSF and restore it to normal levels. This strategy maintains safe and controlled levels of G-CSF, consequently maintaining a pool of neutrophils capable of fighting infections.
“We aren’t proposing to eliminate G-CSF, but to keep it at levels within the normal range. That way we can preserve the normal defense function of these white blood cells but stop them from becoming over-aggressive to lung tissue and other body tissues,” Anderson said.
“This would be the first ever strategy that would not only treat the lung disease but the co-associated medical conditions at the same time. If successful, this has the potential to benefit the millions of people who suffer this terrible disease,” Hibbs said.




