Lung Cancer More Common in COPD Patients, Japanese Study Finds
Written by |
Although lung cancer development is unpredictable, patients with chronic obstructive pulmonary disease (COPD) appear more likely to have the cancer and a worse prognosis compared with the general population, a Japanese study has found.
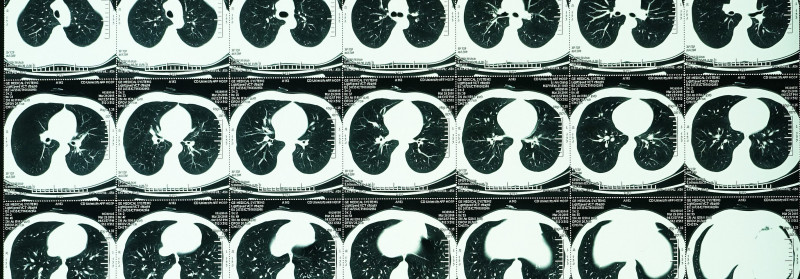
Annual computed tomography (CT) screens may help with the early detection and treatment of this type of cancer in COPD patients, researchers noted.
The study, “The Incidence and Risk Analysis of Lung Cancer Development in Patients with Chronic Obstructive Pulmonary Disease: Possible Effectiveness of Annual CT-Screening,” was published in the International Journal of Chronic Obstructive Pulmonary Disease.
COPD is associated with an increased lung cancer risk, even among non-smokers. Although smoking and emphysema, a severe type of COPD, are known to be risk factors for the cancer, few other reliable predictors have been identified.
In the study, researchers assessed lung cancer and mortality rates in a group of Japanese COPD patients admitted to the Yamagata University Hospital from January 2014 to January 2020. They also explored potential risk factors for the development of the cancer in these patients.
A total of 224 COPD patients, 40 and older, with a history of smoking at least 10 pack-years were included in the analysis. Pack-years is a composite measure of cigarette smoke exposure that takes into account the number of 20-cigarette packs smoked daily and the number of years smoking. For instance, 10 pack-years indicate a person has been smoking a 20-cigarette pack daily for 10 years.
The mean average age of patients was 70.4 years with a mean of 50.7 pack-years, which is equivalent to smoking one 20-cigarette pack daily for 50.7 years. Most patients (214 or 95.5%) were men. Patients were followed for a median period of 4.58 years.
During follow-up, 19 patients developed lung cancer, corresponding to a incidence rate of 1.85% per year.
Consistent with previous studies, COPD patients who developed lung cancer — compared with those who did not — had more severe emphysema, as assessed by scores on chest CT scans, and more severe airflow obstruction, according to GOLD classification.
Moreover, the group of patients who developed lung cancer had a higher average number of pack-years (62.7 vs. 49.6) and a higher proportion of current smokers (31.6% vs 11.2%) compared with the non-cancer group.
Seven (36.8%) patients in lung cancer group and 11 (5.4%) in the non-cancer group died during follow-up. Two deaths (11.1%) were directly attributed to the cancer.
Of the 12 patients diagnosed with lung cancer by tissue analysis, six had adenocarcinoma, three had squamous cell carcinoma, two had small cell lung cancer (SCLC), and one had non-small cell lung cancer (NSCLC).
Both instances of SCLC were detected at advanced stages and the patients died during follow-up, one from lung cancer and another from pneumonia. In contrast, NSCLC was detected early and successfully treated.
Of the seven patients clinically diagnosed with lung cancer, five died during follow-up, including one from the cancer, one from pancreatic cancer, and one due to poor lung function.
In a risk analysis, both severe emphysema and current smoking were significant predictors of lung cancer development.
“In patients with COPD, the incidence of lung cancer is higher, and the development of lung cancer leads to a worse prognosis,” the researchers wrote.
“Since lung cancer development is unpredictable, attention should be paid to all patients. Annual CT screening might be useful in diagnosing lung cancer earlier … and providing appropriate treatment,” they wrote.
The study was limited by its small sample size, observational nature, and relatively short follow-up time. Based on these limitations, the findings “should be validated by a new prospective study with an expanded sample size,” the researchers wrote.




