$2.8M NIH Grant Will Fund Study of Carbon Dioxide Impact in COPD

The National Institutes of Health (NIH) has awarded Albany Medical College, in New York, a $2.8 million, five-year grant to study how carbon dioxide and metabolism impact people with chronic obstructive pulmonary disorder (COPD).
COPD, affecting more than 16.4 million people in the U.S. alone, is a group of chronic inflammatory lung diseases in which the airways become blocked, leading to coughing with mucus and shortness of breath.
Impaired lung function in COPD can alter carbon dioxide levels in the body and affect metabolism. This in turn can contribute to complications like muscle weakness, which can further reduce lung muscle function, limit walking, and increase exacerbations, or episodes of sudden disease worsening. Muscle weakness also leads to associated hospitalizations, and to worse clinical outcomes and quality of life.
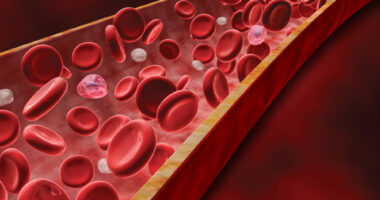
“People with COPD frequently have high levels of carbon dioxide in their blood as well as muscle dysfunction — that is, a loss of muscle strength and endurance — that’s associated with metabolism,” Ariel Jaitovich, MD, a pulmonologist in Albany Med’s division of pulmonary and critical care medicine, said in a press release. Jaitovich also is an associate professor in the departments of medicine and molecular and cellular physiology at Albany Medical College.
Jaitovich and his team will use the funding, awarded by the NIH’s National Heart, Lung, and Blood Institute, to investigate the role of an enzyme called succinate dehydrogenase (SDH) on COPD.
This enzyme is normally found within mitochondria — the small cell compartments that use glucose (sugar) as fuel to produce energy. Mitochondria are found in large amounts in muscle cells, which typically require a great deal of energy to perform their function. SDH is one of the enzymes involved in energy metabolism, a process that releases carbon dioxide as a byproduct, which is then eliminated from the body through respiration.
Studies suggest a reduction in SDH production and function underlies alterations to energy production and muscle impairment in COPD. The team will use animal models to understand the effects of elevated carbon dioxide on metabolism and muscle weakness in COPD.
“We hope to learn how metabolism contributes to the long-term effects of COPD-driven muscle dysfunction, which could eventually lead to the development of drugs that improve the quality of life for those suffering from this disease,” added Jaitovich, who has been piloting NIH-funded studies on COPD since 2016.