CPAP Use May Lower COPD Flare Risk in Patients With Sleep Apnea
Fewer acute exacerbations, better lung function seen with year of regular use
People with chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) may experience fewer acute disease exacerbations if they regularly use noninvasive ventilation at night, a small study in Greece reported.
“Good” nighttime use of continuous positive airway pressure (CPAP), a type of noninvasive ventilation, also aided lung function in COPD patients with OSA, its researchers noted.
The study, “Effect of compliance to continuous positive airway pressure on exacerbations, lung function and symptoms in patients with chronic obstructive pulmonary disease and obstructive sleep apnea (overlap syndrome),” was published in The Clinical Respiratory Journal.
Ideal CPAP use for obstructive sleep apnea is four or more hours each night
COPD occurs when the lungs and the airways become inflamed, causing breathing problems that tend to worsen over time. A sudden worsening of disease symptoms, called an acute exacerbation, is also known and can require hospitalization.
People with overlap syndrome, or COPD as well as OSA, are more likely to experience episodes of acute exacerbation when their OSA is left untreated.
OSA occurs when the airways become partly or fully blocked, and breathing stops and starts repeatedly during sleep. Many with OSA need use a CPAP machine to help them breathe better while they’re asleep.
A CPAP machine is a small, portable device that blows air at a constant pressure via a hose into a mask worn over the nose. The pressurized air helps keep the airways open during sleep.
A research team largely at Democritus University of Thrace investigated whether following a nighttime schedule for CPAP correctly and consistently brought additional benefits to people with overlap syndrome.
The study included 59 people (54 men and five women) with stable COPD and newly diagnosed with OSA, who began treatment with CPAP at a center. According to the researchers, all were “treated according to the latest COPD and OSA guidelines.”
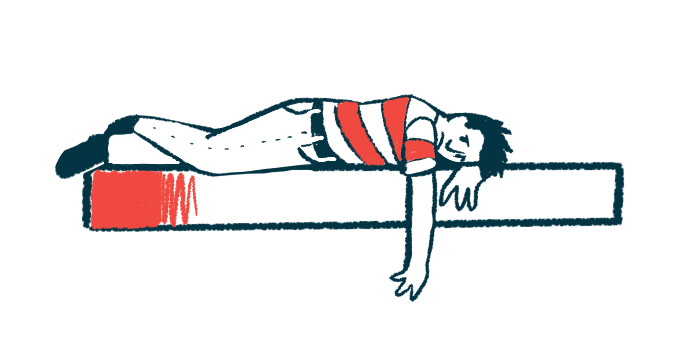
About one year into treatment, 29 patients showed good compliance, used their CPAP device for at least four hours each night (average of 5.5 hours) on at least 70% of all nights. The other 30 patients showed poor compliance, using their CPAP machine an average of 36 minutes each night.
At study entry (a baseline measure), the mean apnea-hypopnea index (AHI) of people with good compliance was about twice that of people with poor compliance (41.7 vs. 20.9 events per hour of sleep). AHI is a measure of the number of times a person experiences apnea (no breathing) or hypopnea (slowed breathing) during the night, divided by the hours of sleep.
After one year of treatment, both those with good and poor compliance saw their mean AHI drop (2.3 and 0 events per hour of sleep). Both also scored significantly better on the Epworth sleepiness scale, which measures daytime sleepiness.
Gain in lung function evident in measures of FEV1, six-minute walking test
However, only those with good compliance saw their lung function get significantly better. They experienced improvements in FEV1, a measure of how much air a person can forcibly exhale in a second after a breath, and total lung capacity, which is the maximum volume of air that can be taken into the lungs.
They also performed better on a six-minute walk test, which measures the distance covered in six minutes, and on the COPD Assessment Test (CAT), which looks at the impact of COPD on a person’s life and how this changes over time.
The number of acute exacerbations also decreased from 17 at baseline to five after one year of treatment in people with good compliance, whereas it remained unchanged, at 15, in those with poor compliance.
Likewise, hospitalizations to treat exacerbations fell over the year in patients with good compliance, from six to none. A decease was also noted in poorly compliant patients, from 12 to five hospitalizations, but this difference did not reach significance.
“In our study, [acute COPD exacerbations] correlated with poor compliance to CPAP treatment and hours of CPAP use,” the researchers wrote.
“This study addresses the central role of compliance to OSA treatment with CPAP on the management of these [COPD] patients, a finding that merits further research,” they added.