Respira’s Remote Device May Aid Timely Care for Lung Disorders
Written by |
A new wearable device can remotely assess lung function in patients and, if federally approved, may help with the early diagnosis and management of chronic obstructive pulmonary disease (COPD), asthma, and COVID-19.
The wearable device, called Sylvee, is worn on the lower part of the rib cage and monitors lung function over time to provide a comprehensive picture of a patient’s condition, without the patient having to leave home.
Developed by Respira Labs, a medical technology company that specializes in respiratory care, the equipment uses small speakers and microphones to “inject” noise into lungs to detect lung resonance changes and unhealthy air trapping. Changes in lung air volume are the basis of traditional lung function tests.
“The device facilitates early diagnosis and management of acute deterioration, which is what respiratory patients must avoid,” Maria Artunduaga, MD, Respira Labs’ founder and CEO, said in a press release. “We provide vital information to doctors and patients so they can make the medical treatment changes earlier and prevent hospitalizations.”
Respira anticipates approval of Sylvee by the U.S. Food and Drug Administration within the next 18 months, and if that happens, the device will be covered by Medicare. The company is seeking to have more than 500 patients participate in a global clinical trial in which it hopes the device can achieve 90% accuracy in detecting air trapping. It also plans to publish in top medical journals by late next year.
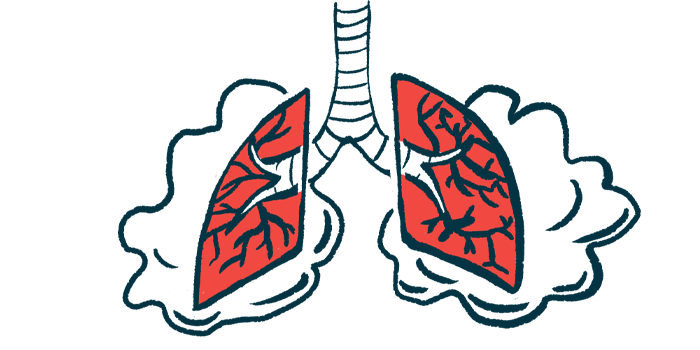
Sylvee works by creating noise in the lung area then gauging the kind of sound subsequently produced. If air is trapped in the lung, the sound that produces is different from the sound resonance created when air is fully expelled. Air trapping is an important and early symptom of respiratory decline.
The Sylvee app uses digital signal processing and artificial intelligence to analyze results. Pulmonologists and primary care physicians can then check those results for lung volume, capacity, and rates of flow and trapped air.
“Well-established science shows that air trapping can be measured with more than 90% accuracy using low-frequency sound,” Artunduaga said. “There is a clear difference in the acoustic resonance spectra of COPD patients versus healthy controls.”
“With more than 100 million Americans affected by COPD, COVID-19 and asthma, and with an aging population, it can be lifesaving to remotely and accurately monitor lung function and discover a problem early enough to avoid serious consequences,” she added. “Our goal is to flag abnormalities early, enable earlier treatment at home and empower patients to manage their own health.”
The technology differs from ultrasounds in that it uses sound to evaluate lung health rather than producing images. The “off-the-shelf” sensors, which uses technology similar to that used in hearing aids, connect to a smartphone application where proprietary algorithms and machine learning transform active sound signals into acoustic resonance markings.
“Sylvee is a tool that could allow us to intervene early when patients with chronic lung conditions develop air trapping, which is a consequence of bronchial spasm or narrowing,” said Luis Peña-Hernández, MD, pulmonologist and intensivist at the Pulmonary, Critical Care & Sleep Disorders Institute of South Florida.
“Patients could receive early medical care that could prevent an exacerbation of asthma or COPD,” he said. “So besides the obvious economic impact, it could be a game changer [in] improving people’s lives, minimizing a disruption in their quality of life, and preventing exacerbations of their chronic lung condition.”
He added that while it’s very likely that such early interventions could improve patient survival, data is still needed to support that hypothesis.