Targeting Fatty Molecules’ Receptors May Aid Lung Repair, Study Shows
Written by |
Activating receptor proteins of prostaglandins (PGs) — fatty molecules with hormone-like effects — restores the regenerative potential of lung cells in cellular models of chronic obstructive pulmonary disease (COPD), a study shows.
This was achieved with iloprost and misoprostol — two compounds that mimic the activity of PGs and are currently used in the clinic for other indications — suggesting that repurposing treatment approaches may help identify potential therapies for COPD.
The benefits were associated with a reversal of COPD-associated lung cells’ abnormalities in the circadian clock, an internally driven 24-hour rhythm, and cell cycle/death signaling pathways.
These findings shed light on the molecular mechanisms behind lung tissue repair and regeneration and such deficits in COPD, which may help to develop or identify new therapeutic approaches.
The study, “A transcriptomics-guided drug target discovery strategy identifies receptor ligands for lung regeneration,” was published in Science Advances.
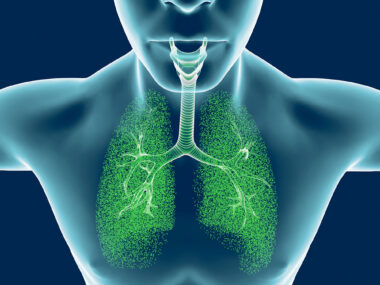
COPD, associated mainly with long-term exposure to irritants such as cigarette smoke, is characterized by excessive airway inflammation and abnormal repair and remodeling of the lung epithelium, the tissue that lines the airways.
This often results in the progressive destruction of the alveoli, the tiny lung air sacs responsible for gas exchange, due to the death of alveolar epithelial cells and the reduced capacity of alveolar epithelial progenitors to counteract this defect.
“As current therapies do not modify the course of the disease, developing new therapeutic strategies aiming at regeneration of tissue is necessary,” the researchers wrote.
Researchers in the Netherlands, Germany, and the U.S. analyzed available gene signatures of lung tissue from people with smoking-associated COPD and mice chronically exposed to cigarette smoke to identify new therapeutic targets in alveolar epithelial progenitors.
The analysis identified 15 potentially targetable genes that showed significantly different activity between COPD samples and healthy samples.
To assess their potential as therapeutic targets to restore lung epithelium regeneration, the team then looked at the effects of compounds known to mimic or block the activity of the molecules coded by those genes.
This was done using lab-grown lung epithelial organoids, or mini-organs, derived from lung cells of mice exposed to cigarette smoke or healthy mice cells exposed in a lab dish to cigarette smoke. Differences in the number and size of alveolar organoids were used to assess alveolar epithelium regenerative capacity.
Results showed that two prostaglandins, PGE2 and PGI2, “had the most profound therapeutic potential in restoring cigarette smoke-induced defects in alveolar epithelial progenitors,” the researchers wrote.
PGs are fatty molecules with hormone-like effects and are most well-known for their effects in the vascular system.
The activity of PTGES2, the gene providing instructions to generate an enzyme responsible for PGE2 production, was significantly reduced in COPD samples relative to healthy samples. In turn, the activity of PTGIR, the gene coding for PGI2’s receptor protein, also known as IP, was significantly increased.
Treating cigarette smoke-exposed mice with either misoprostol — a compound that mimics PGE2 — or iloprost, which mimics PGI2, significantly increased the number of subsequently grown alveolar organoids, relative to no treatment.
Misoprostol, marketed under the brand name Cytotec, is used to treat stomach ulcers. Iloprost, sold as Ventavis, is used to treat high blood pressure in lung arteries and was previously shown to improve clinical outcomes in COPD patients.
These beneficial effects were associated with the activation of EP4, a PGE2 receptor protein, and IP and a correction of alveolar epithelial progenitor cell abnormalities in terms of circadian clock and cell cycle/death signaling pathways.
These results highlight that molecules mimicking the activity of PGE2 and PGI2 “protect alveolar epithelial progenitor function from the effects of [cigarette smoke] exposure,” including disruptions in the circadian clock, the researchers wrote.
As such, the data “provide promising therapeutic strategies to specifically address defective lung repair in respiratory diseases, in particular, targeting EP4 and IP receptors,” the team wrote.
In an accompanying study published in the same journal, researchers at University of Michigan, wrote that “additional work is necessary to further validate the regenerative effects of [PGs] in more demanding models of chronic lung diseases.”
Future research should also focus on better understanding the “mechanisms and significance of [PG-mediated] regulation of molecular targets such as circadian clocks,” they wrote.