OR Nurses, Exposed to Workplace Irritants, at Greater Risk for COPD
Written by |

Female nurses who worked in operating rooms (ORs) for 15 years or more are up to 69% more likely to develop chronic obstructive pulmonary disease (COPD) than those who never served in an OR, according to a large-scale study from the Boston University School of Public Health (BUSPH).
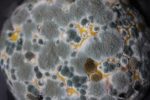
Causing that increased risk, the study found, was exposure in the OR to inhaled workplace irritants such as disinfectants and surgical smoke.
“Our results, based on data from a large cohort [group] of nurses, show that long-time occupational exposure to these agents in operating rooms leads to a significantly higher risk of developing COPD,” Wubin Xie, the study’s first author, of the BUSPH’s department of global health, said in a press release.
The study, “Association of Occupational Exposure to Inhaled Agents in Operating Rooms With Incidence of Chronic Obstructive Pulmonary Disease Among US Female Nurse,” was published in the journal JAMA Network Open.
The primary factor associated with the development of COPD is tobacco smoking, but increasing evidence suggests occupational exposure is another contributor to this chronic inflammatory disease of the lungs.
In a healthcare setting, it is common for workers to be exposed to disinfectants and surgical smoke — a visible gaseous by-product that comes from lasers used to cut tissue, instruments used for electrical cauterization, and ultrasonic scalpel dissection.
Although contact with these hazardous materials varies by job type, studies suggest that operating room or OR nurses have the highest level of disinfectant use, and are commonly exposed to surgical smoke.
“Smoke-generating laparoscopic surgery is performed in a broader range of procedures, and protective surgical masks, such as the N95 mask, cannot block the small particulates in surgical smoke,” Xie said.
While the irritant properties of chemicals in disinfectants and surgical smoke have been established for some time, the long-term association with employment in an OR and the risk of COPD remains unknown.
“One of the inherent challenges with assessing the health risks of disinfectants and surgical smoke is that it is difficult to measure exposure with precision over an extended period of time and among a large population,” Xie said.
Now, researchers at BUSPH collaborated with colleagues at Harvard Medical School, Brigham and Women’s Hospital, and Inserm National French Institute of Health & Medical Research to investigate further — focusing on nurses working in U.S. hospitals.
“To our knowledge, the association of OR employment history with COPD has not been investigated in a large population,” the team wrote.
Data were collected from the Nurses’ Health Study (NHS), an ongoing study of more than 121,000 female nurses in the U.S., ages 30–55. Study participants have completed health-related questionnaires every two years since 1976.
Selected information on COPD incidence and OR employment history was extracted from a subset of 75,011 nurses working in U.S. hospitals in 1984, who were followed until 2000.
While the study reflected working conditions in the 1980s, the researchers noted that “that the findings are still relevant to current working conditions for a few reasons,” including the increased use of disinfectants to prevent infections, and the lack of evidence that surgical smoke has been reduced.
Indeed, according to the team, “smoke-generating minimally invasive surgery has been performed in an increasingly diverse array of contexts and is now considered the standard of care for a wide spectrum of general surgical procedures.”
Because direct exposure could not be measured, the researchers used the nurses’ OR employment duration as a proxy to determine their exposure to inhaled substances. Nurses were divided into three groups, depending on the time they worked in the OR: less than five years; five to 14 years; and 15 years or more.
For comparison purposes, nurses with jobs outside the OR, such as those working in administration, education, outpatient or inpatient care, or in emergency departments, also were assessed.
The analyses also took into account factors that might influence the results, such as ethnicity, age, U.S. region, smoking status, amount smoked, and body mass index (BMI), which is a body fat measure.
The nurses, all female, had a mean age of 50.5 in 1984. Nearly all (96.9%) were non-Hispanic white, with the remaining 3.1% identified as other. Nearly half (44.9%) reported they had never smoked, and 13.4% were considered obese.
A total of 71% never worked in the OR. Of the 29% who did, 20% reported working there for less than five years, 6% for 5–14 years, and 3% for 15 years or more.
During the 16-year follow-up period, there were 1,091 recorded cases of COPD, with higher rates associated with longer OR employment history.
Without adjustments, COPD incidence among nurses working less than five years and 5–14 years in the OR were similar. After adjusting data for age, any OR employment was found to be associated with a 16% increased risk of COPD than no OR employment.
Compared with participants with no OR history, those who reported working there for 15 years or more had a 46% increased risk of developing COPD after adjusting for all factors. While there was a significant trend of increased risk as the number of years in the OR increased, a strong association was only found for nurses who worked in the OR for 15 years or more.
Further subdividing nurses based on job type revealed that, compared with those working in administration, education, or a non-nursing job, those working in outpatient care had a 24% increased risk of developing COPD. Likewise, nurses working in the emergency department or in inpatient care had a 31% increased risk of having COPD.
The researchers noted that these nurses had “increased exposure to disinfectants but no or little exposure to surgical smoke.”
Notably, the strongest association — corresponding to a 69% increased risk of COPD — was seen among nurses who had worked in the OR for 15 years or more.
“This difference may be explained by a synergistic effect of surgical smoke and disinfectant exposure or a higher level of exposure to surgical smoke and/or disinfectants in this particular type of nursing job,” the researchers wrote.
Similar results were found after adjusting data for physical activity, diet quality, secondhand smoke exposure, spouse’s educational level, and when those with a history of chronic illnesses were excluded.
No connection between OR employment and COPD was seen among nurses who currently smoke. Although COPD risk was higher for former smokers, the association was not significant for nurses who worked 5–14 years in the OR. Yet, for those with 15 years or more of OR experience, COPD risk was 97% higher than among those who never smoked.
“In this large prospective cohort study of US female nurses, OR employment for 15 or more years assessed in 1984 was associated with an increased risk of incident COPD over 16 years of follow-up,” the investigators concluded.
Because there is greater diversity among nurses nowadays, “additional studies with more detailed and recent exposure assessment are needed to better understand COPD risk among hospital staff exposed to toxic agents in the operating room,” said Andrew Stokes, PhD, the study’s senior author and an assistant professor of global health at BUSPH.